Interventional Radiologists: Pioneers of Minimally-Invasive Treatments for Peripheral Vascular Disease
Homer Stevens could not walk far because his legs would tire out quickly and his toe was black, swollen and very painful. His quality of life suffered. His podiatrist suggested that he might have a circulation problem and recommended he get tested for Peripheral Vascular Disease (PVD).
What is Peripheral Vascular Disease
Click here to watch Dr. Matthew Dicker: What is Peripheral Vascular Disease? on YouTube.
PVD or PAD (Peripheral Arterial Disease), which is also known as atherosclerosis or hardening of the arteries, affects the blood vessels outside of the heart and brain. Scar tissue and cholesterol build up in the arteries and form a plaque that eventually causes blockages. These blockages are serious because they decrease or even stop blood flow to important parts of the body, such as the arms and legs. The blockages from PVD limit the amount of oxygen and nutrients the muscles receive, which leads to pain.
Local Interventional Radiologists Matthew Dicker, M.D., and Ben Paxton, M.D., are blood vessel experts who diagnose and treat PVD, which is a serious public health issue that affects as many as twenty percent of Americans 65 and older.
Dr. Dicker said, “When blood flow to the extremities decreases, the patient may have several different symptoms. Prior to that time, they may not have any symptoms and attribute their pain to the aging process. When it does become symptomatic, patients most often develop intermittent claudication. This is when pain, burning, tiredness or fatigue is felt in the calf while exercising or walking and stops as soon as the patient stops the activity.”
“When the blockage is more severe, blood flow cannot meet the requirements of the body to heal sores or wounds, so wounds may heal very slowly or not at all which can lead to infection and, later, amputation,” added Dr. Dicker.
PVD is a systemic disease, which means that it can affect the entire body. diabetes and hypertension are risk factors for PVD, and once someone has PVD, he or she is at increased risk of developing heart disease, aortic aneurysms and stroke.
“Diagnosis starts with obtaining a comprehensive patient history and physical examination, which includes assessing the pulses of the legs. Testing ranges from non-invasive modalities such as the Ankle-Brachial Index (ABI), which is used to compare the blood pressure between the arms and legs, Magnetic Resonance Angiogram (MRA), CT Angiogram (CTA), Ultrasound, or the semi-invasive angiogram,” said Dr. Dicker.
Initial treatment options for PVD range from lifestyle changes such as smoking cessation, weight loss, exercise or cholesterol-lowering medications. Interventional radiology treatments such as angioplasty and stenting—which were pioneered by interventional radiologists—and atherectomy or stent grafts are all image-guided, minimally-invasive options that might be considered as well.
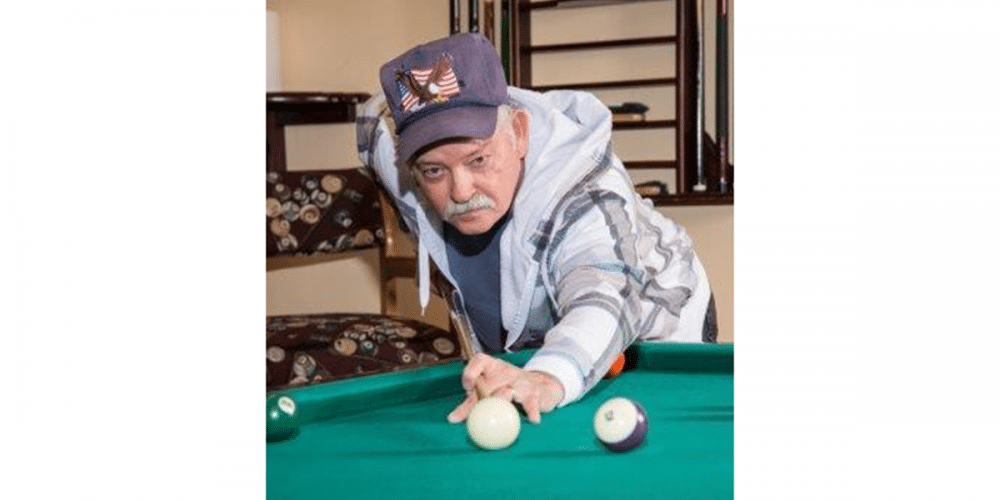
Before Homer Stevens had his stents placed, his blood flow was poor, and walking even short distances was difficult. “I couldn’t even get out and work in the yard for periods of time because my legs would tire out,” said Stevens. Today, Homer says he has a new lease on life. He can go hunting with his brother, take hikes and play pool because it no longer hurts him to stand for long periods of time or to bend over. He encourages his friends to see their doctors and educates them about paying attention to all symptoms, especially in older age. “I try to steer them in the right direction because I am excited about what Dr. Dicker has done for me.”
If you have a family history of arterial blockages such as PVD, PAD or hardening of the arteries, or questions about any symptoms you may be experiencing, please discuss it with your primary care provider or consult a specialist such as a cardiologist, or contact the interventional radiologists at Vascular and Interventional Specialists of Prescott by calling (928) 771-8477.
Vascular & Interventional Specialists of Prescott was formed in 2010 by a group of subspecialty radiologists that perform numerous minimally-invasive, low-risk procedures using the tools of our trade for guidance—x-ray, ultrasound, CT scan, and MRI. The team’s goal is to educate patients and medical communities, while also providing safe and compassionate health care, with rapid recovery times and low risk of complications.