Deep vein thrombosis (DVT) is a medical condition characterized by the formation of a blood clot in a deep vein, most commonly in the legs. These clots can obstruct blood flow, leading to swelling, pain, and potentially more severe complications if the clot dislodges and travels to the lungs, causing a pulmonary embolism.
Recognizing who is at greater risk for DVT is crucial for prevention and early intervention. Keep reading below to learn more.
What Causes Deep Vein Thrombosis (DVT)?
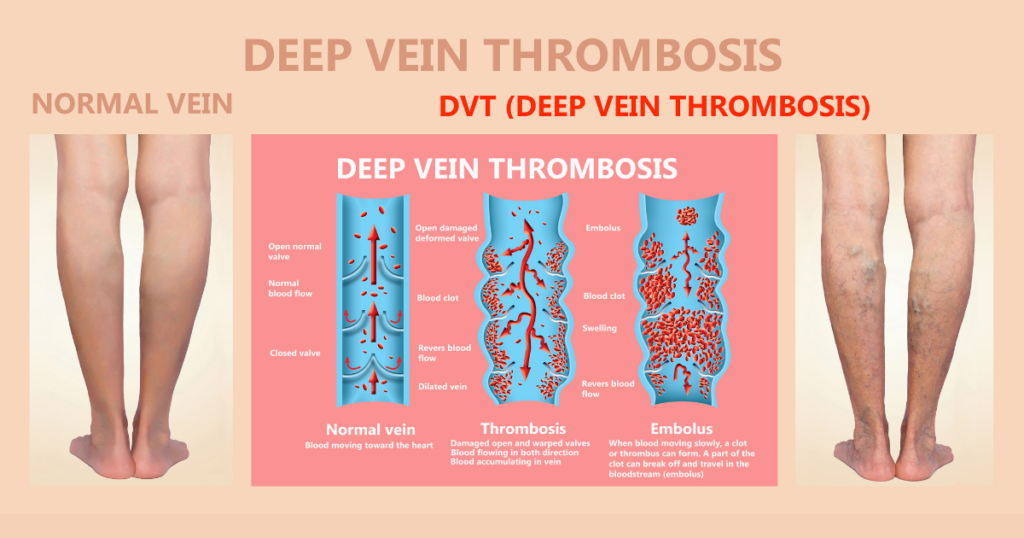
When a blood clot forms in a certain vein deep inside the body, it causes what health professionals call deep vein thrombosis.
The development of deep venous thrombosis is typically attributed to a combination of factors that affect blood flow and clotting mechanisms. These include:
- Immobility: Prolonged periods of inactivity, such as bed rest during hospitalization, long flights, or sedentary lifestyles, can slow blood flow in the legs, increasing the risk of blood clot formation.
- Injury or Surgery: Trauma to deep veins from injury or surgical procedures can damage blood vessels, creating a site for clot formation.
- Medical Conditions: Certain medical conditions, such as cancer, heart failure, inflammatory bowel disease, and clotting disorders, can predispose individuals to DVT.
- Hormonal Factors: Hormone replacement therapy, birth control pills, and pregnancy can elevate levels of clotting factors, increasing the risk of DVT.
- Genetics: A family history of DVT or inherited clotting disorders can make one more susceptible to developing blood clots.
- Age: The risk of DVT increases with age, particularly in individuals over 60.
Blood Clot Formation
The formation of blood clots is a vital process that stops bleeding and initiates healing after an injury. However, inappropriate clotting within veins can lead to DVT. The clotting process involves vascular spasm, platelet plug formation, and the coagulation cascade, which stabilizes the clot.
Factors such as venous stasis, endothelial injury, and hypercoagulability contribute to abnormal clot formation. Highlighting the importance of regular movement, professionally guided medication, and lifestyle changes can prevent blood clots.
[Also Read: How to Prevent DVT – 5 Tips From a Vein Specialist]
Who Is More Prone to DVT?
Certain groups of people are at a higher risk of developing deep vein thrombosis. These include:
Individuals with a History of DVT or PE
Those who have previously experienced DVT or pulmonary embolism (PE) are at a higher risk of recurrence. The presence of a prior clot suggests an underlying predisposition, whether due to lifestyle, medical conditions, or genetic factors.
Moreover, genetic predisposition plays a significant role. Individuals with a family history of DVT are also at risk
People with Certain Medical Conditions
Several medical conditions markedly elevate the risk of DVT. Cancer patients, particularly those undergoing chemotherapy, face a higher risk due to both the malignancy itself and the treatments that often impair blood flow and clotting mechanisms.
Additionally, conditions like heart disease, which can affect circulation, lung disease, which can reduce blood oxygen levels and contribute to clot formation, and inflammatory diseases like rheumatoid arthritis and inflammatory bowel disease, which can increase inflammation and blood clotting, are significant risk factors.
Post-Surgical Patients
Post-surgical patients, especially those who have undergone major operations such as hip or knee replacements, are at increased risk of DVT. The reasons include prolonged immobility during and after surgery, which slows blood flow in the veins, and direct injury to blood vessels during the procedure, which can initiate clot formation.
Surgeries involving the abdomen or pelvis also pose a high risk due to potential disruption of blood flow in these areas.
Pregnant Women
Pregnancy induces physiological changes that elevate DVT risk. The increased pressure on veins in the pelvis and legs, along with higher levels of clotting factors and decreased levels of natural anticoagulants (blood thinners) in the blood, contribute to this risk.
Additionally, the post-partum period is particularly critical, as the body adjusts from the hypercoagulable state of pregnancy back to normal.
Women on Hormonal Therapy
Women using oral contraceptives or undergoing hormone replacement therapy (HRT) are more prone to DVT. These hormonal treatments can increase the levels of certain clotting factors and reduce the levels of anticoagulants in the blood.
Obese Individuals
Obesity is a significant risk factor for DVT. Excess body weight increases pressure in the veins of the legs and pelvis, which can hinder blood flow and promote clot formation.
Additionally, obese individuals often have other comorbidities, such as hypertension and diabetes, which further elevate the risk.
Smokers
Smoking adversely affects blood clotting and circulation. The chemicals in tobacco smoke damage the lining of blood vessels, making them more susceptible to clot formation.
Moreover, smoking also reduces blood oxygen levels, which can contribute to conditions favorable for DVT development.
People with Sedentary Lifestyles
A sedentary lifestyle, especially during long-distance travel or prolonged periods of sitting, can significantly increase the risk of DVT. Lack of regular movement slows down blood flow in the legs, leading to stasis, which is one of the critical components of clot formation.
Individuals who work in occupations requiring long hours of sitting or standing still without movement are particularly vulnerable.
Older Adults
Age is a well-documented risk factor for DVT. As individuals age, their veins and valves may weaken, leading to poor circulation and an increased tendency for blood to pool and clot.
Those over 60 are especially susceptible, with the risk doubling every decade after the age of 50.

Is a DVT an Emergency?
Yes, deep vein thrombosis can be an emergency, particularly if there is a risk of the clot dislodging and traveling to the lungs, causing a pulmonary embolism (PE).
Pulmonary embolism is a life-threatening condition that requires immediate medical attention. Symptoms of PE include sudden shortness of breath, chest pain, rapid heart rate, and coughing up blood. If any of these symptoms occur, it is crucial to seek emergency medical care.
What Is the Survival Rate of Deep Vein Thrombosis?
The survival rate of DVT can vary based on the severity of the condition and the timeliness of treatment. With prompt and appropriate treatment, the prognosis for DVT is generally good. However, untreated DVT can lead to serious complications, including pulmonary embolism, which can be fatal. The survival rate for those with DVT alone is quite high with treatment, but complications such as PE significantly reduce the survival rate.
Does Deep Vein Thrombosis Go Away?
With proper medical treatment, deep vein thrombosis can resolve over time. Treatment typically involves blood thinners, which help to prevent further clotting and allow the body to gradually dissolve the existing clot. In some cases, thrombolytic therapy or surgical intervention may be necessary to remove the clot. Additionally, lifestyle changes, such as increased physical activity, weight management, and smoking cessation, are important for preventing recurrence.
Seek Professional Care for Your Vascular Health
Deep vein thrombosis is a condition that necessitates awareness and proactive management. Recognizing the risk factors and understanding the causes can aid in prevention and early detection. With proper care, the risks associated with DVT can be significantly mitigated, ensuring better health outcomes.
If you are concerned about your risk for deep vein thrombosis or are experiencing symptoms that could indicate DVT, don’t wait. Schedule a consultation with the Vascular & Interventional Specialists of Prescott (VISP). Our experienced team can provide comprehensive evaluations, advanced diagnostic testing, and personalized treatment plans to help you manage and prevent DVT.
Take control of your vascular health today—contact VISP to book your appointment.
