What Is The Best Treatment for PVD in Legs?

Peripheral vascular disease is a circulatory disease that affects the blood vessels in the extremities, such as the feet and legs. This condition occurs when a blood vessel becomes narrowed, blocked, or spasmed, resulting in reduced blood flow and potential complications.
PVD can be a slow-progressing disorder. Here’s the good news though: timely treatment and intervention can greatly improve the quality of life of those affected.
In this article, we’ll discuss the signs, symptoms, causes, risk factors, and explore the best treatment for PVD in legs to improve your condition and overall quality of life.
Understanding PVD: Causes, Symptoms, and Risk Factors
Peripheral vascular disease (PVD) is a complex circulatory condition that can have serious consequences for your health. It affects arteries, arterioles, and veins. All of these contribute to the body’s complex vascular systems. Capillaries, the smallest blood vessels, link these systems together.
While PVD can occur anywhere in the body, it most commonly affects the extremities, such as the legs. It can cause discomfort, reduced mobility, and complications such as ulcers and injuries.
Understanding the symptoms, risk factors, and causes is important for early diagnosis, prompt PVD treatment, effective management, and better overall health.
Causes of PVD
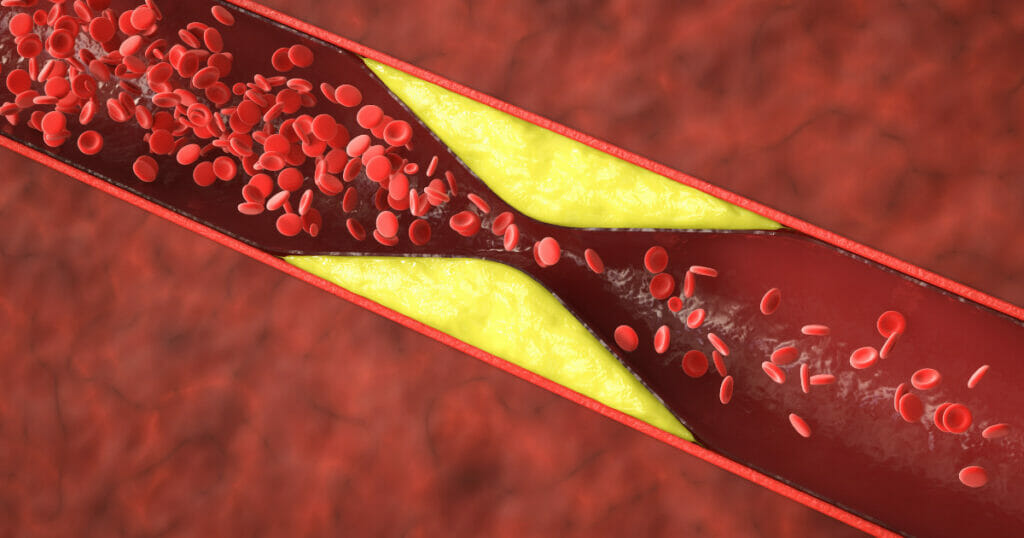
PVD’s leading cause is atherosclerosis, often referred to as the “hardening of the arteries”. This is caused by the gradual accumulation of calcium, cellular wastes, and fatty substances on the inner walls of arteries.
Over time this buildup causes plaques, which narrow the vessels and reduce blood flow to various parts of the body, especially the extremities. Blood vessel constriction can reduce oxygen and nutrient delivery to tissues, leading to fatigued legs, cramping pain, and non-healing ulcers.
Risk Factors of PVD
Several risk factors are associated with increased susceptibility to peripheral vascular disease (PVD) and peripheral arterial disease (PAD). It is important to identify these risk factors for both prevention as well as effective symptom management.
- Smoking: Smoking is a significant risk factor for PVD. It damages the blood vessels, causes atherosclerosis, and accelerates the progression of the disease. Smokers have a greater risk of developing peripheral vascular disease and experiencing its symptoms earlier than those who do not smoke.
- Diabetes: People who have diabetes are at a greater risk of developing PVD. Elevated blood glucose levels can damage the blood vessels and make them more susceptible to atherosclerosis and other circulatory issues.
- Age: PVD is a disease that primarily affects those over 60. As age advances, the risk of developing PVD increases.
- Prior Coronary Artery Disease: People who have had coronary artery diseases in the past are at a higher risk of developing PVD. Both conditions have similar risk factors and mechanisms.
- Obesity: Living with obesity can lead to atherosclerosis, and increase the risk of PVD. Maintaining a healthy weight is essential for vascular health.
- Sedentary Lifestyle: Lack of physical activity may lead to PVD and other health issues. Regular exercise helps to improve blood circulation and reduces your risk of developing vascular disorders.
- High Blood Pressure (Hypertension): Hypertension causes blood vessels to be more vulnerable to damage and atherosclerosis. Uncontrolled high blood tension can worsen PVD symptoms.
- High Blood Cholesterol (Hypercholesterolemia): Elevated levels of LDL (low-density lipoprotein) cholesterol, often referred to as “bad” cholesterol, contribute to the development of atherosclerosis and PVD.
- Family History: Genetic factors can influence PVD risk. Individuals with a familial history of PVD, heart disease, or related conditions have a higher risk of developing the disorder.
- Medical History: A history of previous strokes, heart attacks, or cardiovascular diseases may increase the risk of PVD as these conditions all share similar causes.
[Related: What Is the Difference Between PAD and PVD?]
Recognizing the Signs and Symptoms
PVD often progresses slowly, and its symptoms can be subtle. The symptoms of PVD can vary widely, making early detection and intervention crucial:
- Rapid leg fatigue during activities.
- Leg and foot cramps, particularly when lying down.
- Hair growth reduction in legs.
- Numbness and tingling sensations in the hands or feet.
- Skin discoloration of the arms and legs, turning reddish-blue or pale.
- Weak or absent pulses in the arms and legs.
- Non-healing wounds or ulcers.
- Muscle discomfort, such as numbness or heaviness in leg muscles.
PVD can lead to intermittent pain, coldness, muscular weakness, and, in severe cases, even gangrene. Understanding these symptoms and risk factors is critical to recognize when treatment may be required.
How is Peripheral Vascular Disease Diagnosed?
Proper diagnosis of PVD involves gathering relevant medical history information, performing a physical exam, and running various diagnostic tests. These may include the following:
- Angiograms
- Ankle-brachial index (ABI) measurements
- Doppler ultrasound flow studies
- Magnetic resonance angiography (MRA)
- Treadmill exercise tests
Healthcare professionals use these tests to assess the severity of PVD and recommend treatment plans accordingly. Regular check-ups and monitoring are crucial in effectively managing PVD and avoiding complications.
Treatment Approaches for PVD
Finding an effective treatment for PVD requires an integrated approach tailored to the individual’s specific condition. Prominent treatment options include:
Lifestyle Changes

Lifestyle changes are an effective first defense against PVD, serving to both decrease risk factors and enhance blood circulation.
Quitting smoking is crucial, as it’s a major risk factor. Cessation programs, medications, and support groups can all assist with quitting smoking successfully.
Engaging in regular exercise, adopting a balanced diet low in saturated fats, maintaining a healthy weight, and controlling co-existing conditions like diabetes and hypertension are important steps. Doctor-recommended walking regimens and leg exercises also help alleviate pain.
Maintaining a healthy weight reduces strain on blood vessels. Heart-healthy diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats have long been recommended to promote cardiovascular health.
Individuals living with PVD should consult healthcare professionals to treat co-occurring conditions like diabetes, high blood pressure, and cholesterol issues.
Medications
Medication plays an integral part in managing PVD symptoms and reducing complications. Common medications include:
- Cholesterol-Lowering Drugs: Statins are commonly prescribed to reduce LDL cholesterol levels, prevent plaque buildup in arteries, and combat atherosclerosis.
- Antiplatelet Agents: Blood thinners, such as clopidogrel or aspirin, prevent platelets from clumping together on top of plaque buildup. This medication is prescribed primarily to help prevent blood clots.
- Blood Pressure Medications: Controlling high levels of blood pressure through medication helps to maintain arterial health.
- Medications for Leg Pain: Cilostazol may improve blood flow and relieve symptoms such as leg muscle pain or fatigue.
- Other medications: Depending on your condition, your doctor may also prescribe medications to manage blood sugar, blood pressure, and other co-occurring conditions.
Minimally Invasive Procedures
Minimally invasive procedures have become an increasingly popular way of managing PVD, providing effective alternatives to traditional surgery. These procedures are performed by interventional radiologists and may include:
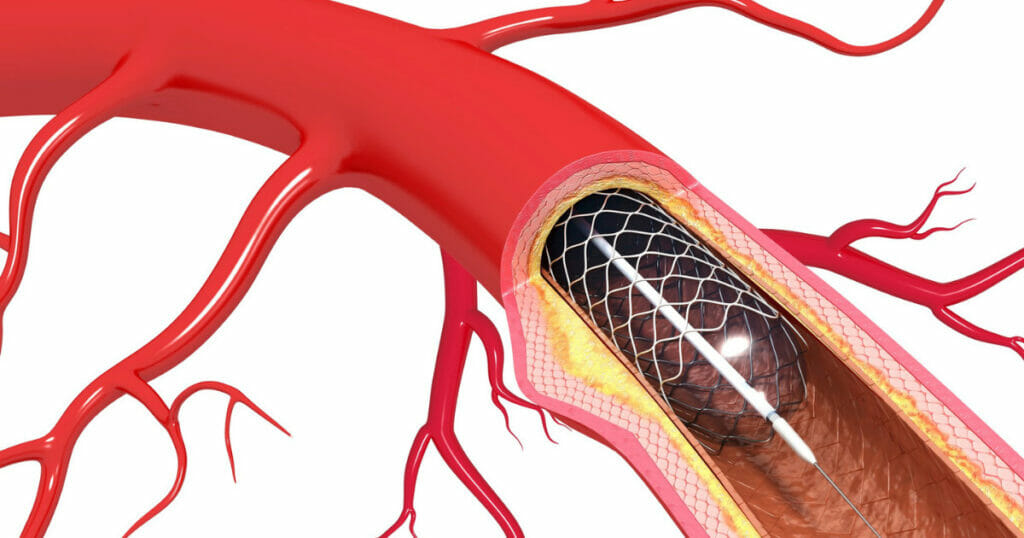
Angioplasty: This minimally-invasive procedure involves inserting a catheter with an inflatable balloon into the blocked artery. The balloon is inflated to widen the artery and improve the blood flow.
In some cases, a stent may be placed to keep the artery open.
Atherectomy: This procedure involves removing plaques from the blood vessel walls to increase blood flow. Atherectomy uses a balloon and a catheter equipped with a tool that cuts plaque to restore blood flow.
Stent Placement: After an angioplasty, or atherectomy, stenting can be done to keep the treated artery wide open. This prevents the narrowing of the vessels treated. Stent placement involves the insertion of a mesh tube (stent) that keeps open treated arteries.
Vascular Bypass Surgery
For severe cases of PVD, surgical interventions may be required to bypass a blocked or narrowed artery and restore circulation more freely.
In severe instances, bypass surgery might even be required; healthy veins or synthetic tubes will be used to redirect blood around these obstructions. This allows blood to circulate more freely and improves circulation.
Get the Best Treatment for PVD In Legs
Peripheral vascular disease is a serious condition that requires prompt attention and appropriate treatment. Patients need to recognize signs, control risk factors, and receive appropriate treatment for PVD in the legs.
Early intervention and adherence to treatment plans can improve the overall quality of life and cardiovascular health of PVD patients.
Consultation with healthcare specialists such as interventional radiologists and vascular specialists can provide customized treatment plans tailored to meet your needs.
At VISP, your vascular health is our priority. If you or someone you know is suffering from possible symptoms of peripheral vascular disease and peripheral artery disease, don’t hesitate to get noninvasive treatments from our interventional radiologists!
Visit us at vispdocs.com, or call 928.771.8477 for more information.
Vascular & Interventional Specialists of Prescott was formed in 2010 by a group of subspecialty radiologists that perform numerous minimally-invasive, low-risk procedures using the tools of our trade for guidance—x-ray, ultrasound, CT scan, and MRI. The team’s goal is to educate patients and medical communities, while also providing safe and compassionate health care, with rapid recovery times and low risk of complications.
